Finite Element Analysis and Thermal Interface Materials in Medical Laser Design
Introduction
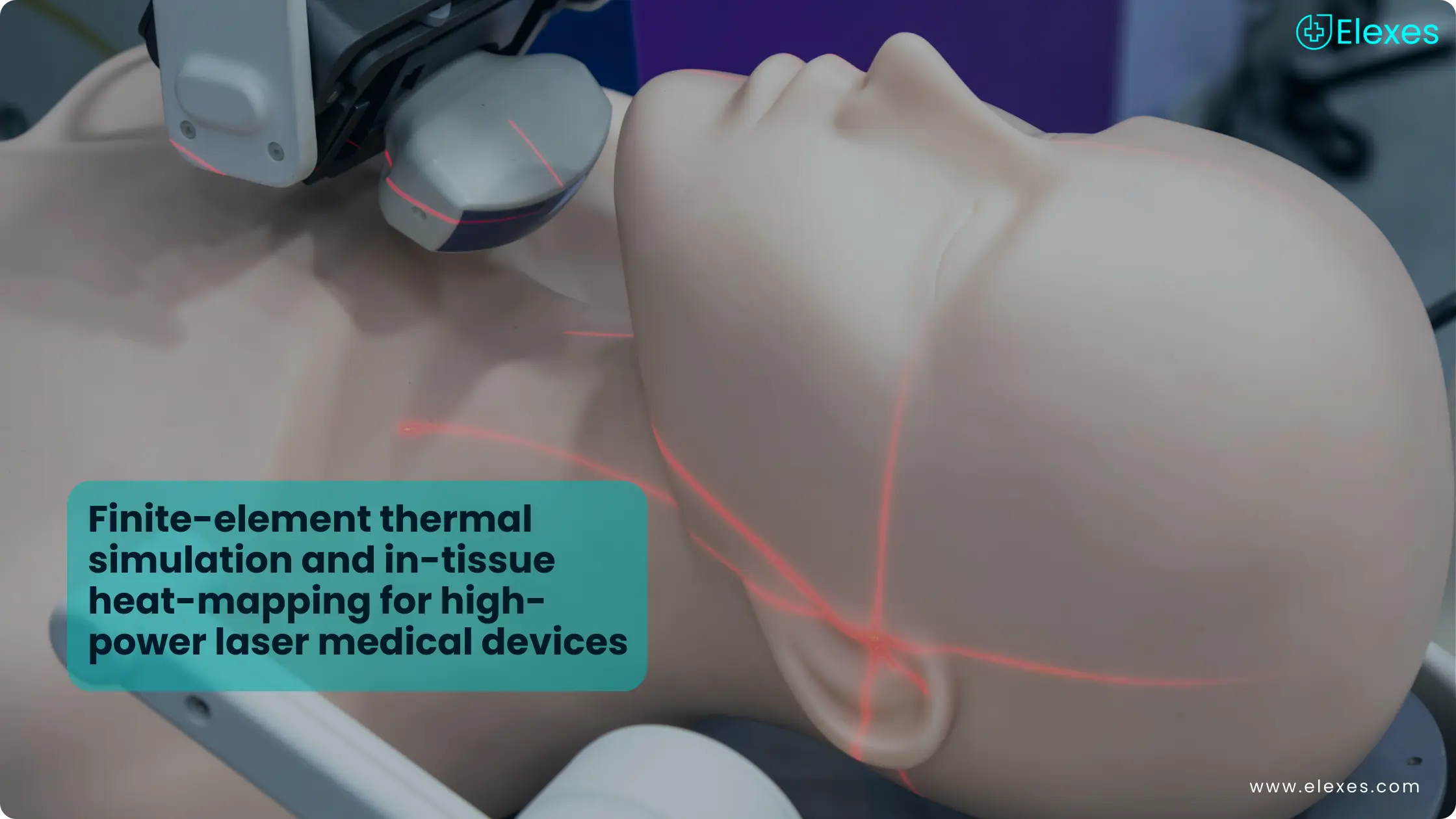
High-power laser systems used in ophthalmic, surgical, and dermatologic devices generate significant heat within laser diodes, optics, and associated electronics during operation. Often, controlled thermal energy is a prerequisite for clinical efficacy, but if overheating is not properly managed, it can affect device performance, patient safety, and regulatory compliance. Effective thermal management and bio-safety planning are therefore critical throughout the design and validation of laser-based medical devices.
Modern development strategies increasingly rely on Finite element analysis to predict heat generation, transfer and dissipation. Alongside this, the correct selection and qualification of Thermal interface materials plays a central role in maintaining safe operating temperatures and minimizing thermal risk.
Finite Element Analysis for Heat Simulation in Medical Lasers
The analysis of finite elements helps engineers understand heat flow, hotspot formation, and cooling efficiency, the creation of hot spots and the efficiency of cooling in laser modules in a detailed manner. The engineers can accurately simulate the influences of conduction, convection and radiation through the structure of the device by breaking down the intricate geometries into tiny elements. In many high-power laser diode assemblies, a significant portion of the overall temperature rise can be attributed to thermal resistance at material interfaces, particularly between the chip, submount, and heat sink.
Published studies on laser diode packaging report interface thermal resistance values on the order of a few tenths of a kelvin per watt, highlighting the importance of interface design and material selection.
In the case of medical laser applications like ophthalmic ablation, dermatologic resurfacing, and surgical cutting or coagulation, Finite element analysis empowers the designers to:
⦿ Predict junction and surface temperature rise under both continuous-wave and pulsed laser operating modes
⦿ Monitor thermal behavior both in steady state and transient conditions
⦿ Assess the impact of Thermal interface materials on overall thermal resistance
This simulation-driven approach allows potential thermal risks to be addressed early in development, reducing costly redesigns and supporting regulatory submissions.
Role of Thermal Interface Materials in Laser Device Safety

Thermal interface materials work by providing the necessary thermal contact between components such as laser diodes, submounts and heat sinks. Common materials include thermal greases, phase-change materials, gap fillers and thermally conductive pads.
In medical laser devices, the selection of Thermal interface materials must consider:
⦿ Thermal conductivity and long-term stability
⦿ Biocompatibility considerations where indirect patient exposure is possible, along with strict cleanliness and contamination control requirements
⦿ Resistance to aging, pump-out and degradation under repeated thermal cycling
⦿ Compatibility with applicable sterilization or high-temperature cleaning processes, particularly for reusable or proximity-to-sterile-field components
When poorly chosen, the interface materials can create hotspots that lead to reduced laser life, and increase the possibility of surface temperatures going over the regulated limits.
IEC 60601-1 Temperature Limits and Thermal Safety Compliance
Medical electrical equipment is covered by IEC 60601-1, the general safety standard of medical devices. This standard defines temperature limits for accessible parts of medical electrical equipment under specified contact conditions and durations, forming a key part of thermal safety evaluation. Laser-based medical devices must comply, which requires close alignment between thermal modeling, physical testing, and documented risk controls.
Designers have to prove that:
⦿ Accessible parts have the temperature below the maximum limit during ordinary use
⦿ Fault situations will not cause an unsafe temperature rise
⦿ Transient thermal excursions are assessed and controlled
Outputs from Finite element analysis, combined with validated Thermal interface materials, provide objective evidence to support compliance with IEC 60601-1 thermal safety requirements.
These evaluations are typically performed in conjunction with risk management activities in accordance with ISO 14971.
In-Tissue Heat Mapping and Experimental Validation
Simulation alone is not sufficient to demonstrate thermal bio-safety. In-tissue heat mapping provides essential empirical validation of predicted thermal behavior.
Common validation methods include:
⦿ Infrared thermography for surface temperature distribution visualization
⦿ Thermocouples for internal temperature rise measurement
⦿ Thermal imaging in operating conditions on tissue phantoms or ex vivo models
A typical validation workflow includes:
⦿ Simulating heat generation and conduction using Finite element analysis
⦿ Predicting temperature rise at device-tissue interfaces
⦿ Testing under representative laser power and duty cycle conditions
⦿ Comparing measured data with simulation results and IEC 60601-1 limits
This combined approach supports both therapeutic effectiveness and the prevention of unintended thermal injury.
Why Thermal Management Matters for Regulatory and Clinical Success

In ophthalmic lasers for retinal photocoagulation, surgery lasers for tissue ablation and dermatologic lasers for skin rejuvenation or hair removal, thermal energy is consciously directed to the affected tissue. Yet, the unintentional heating of the adjacent tissues or device surfaces poses a major safety hazard.
The use of Finite element analysis in thermal management, the constant testing of Thermal interface materials, compliance with IEC 60601-1 temperature limits and thorough in-tissue validation are all necessary for:
⦿ Regulatory acceptance
⦿ Patient safety
⦿ Long-term device reliability
⦿ Consistent clinical performance
Conclusion
Thermal performance in high-power laser medical devices cannot be treated as a stand-alone engineering detail. It has a direct impact on device safety, long-term reliability, and the ability to meet regulatory expectations. Using finite element analysis early in the design process helps teams understand how heat is generated, transferred, and dissipated, while thoughtful selection of thermal interface materials plays a key role in controlling interface resistance and maintaining stable operating temperatures over time.
When these design decisions are backed by experimental validation and aligned with IEC 60601-1 temperature limits and risk management practices, they create a strong and defensible basis for both clinical performance and compliance. Addressing thermal behavior early in development reduces the need for late-stage redesigns and also leads to more predictable real-world performance and, ultimately, safer outcomes for both patients and clinicians.